Documenting your ASC COVID Emergency Response
Written by: Debra Stinchcomb MBA, BSN, RN, CASC
Ambulatory surgery centers (ASCs) have experienced many changes within the past few months. In response to COVID-19, many ASCs had to close or decrease their cases and are now in the process of reopening or ramping up their operations again. During this phase, ASC leaders are undoubtedly dealing with a number of challenges, including navigating supply shortages, tackling HR issues, and working to implement new policies based on rapidly changing recommendations.
The dynamic environment ASCs find themselves in as a result of COVID-19 has important implications from a compliance perspective, with a heightened need for clear and comprehensive documentation to meet the requirements for risk management and survey purposes. Below are some key compliance areas for ASC leaders to focus on during the pandemic.
Emergency Preparedness Requirements
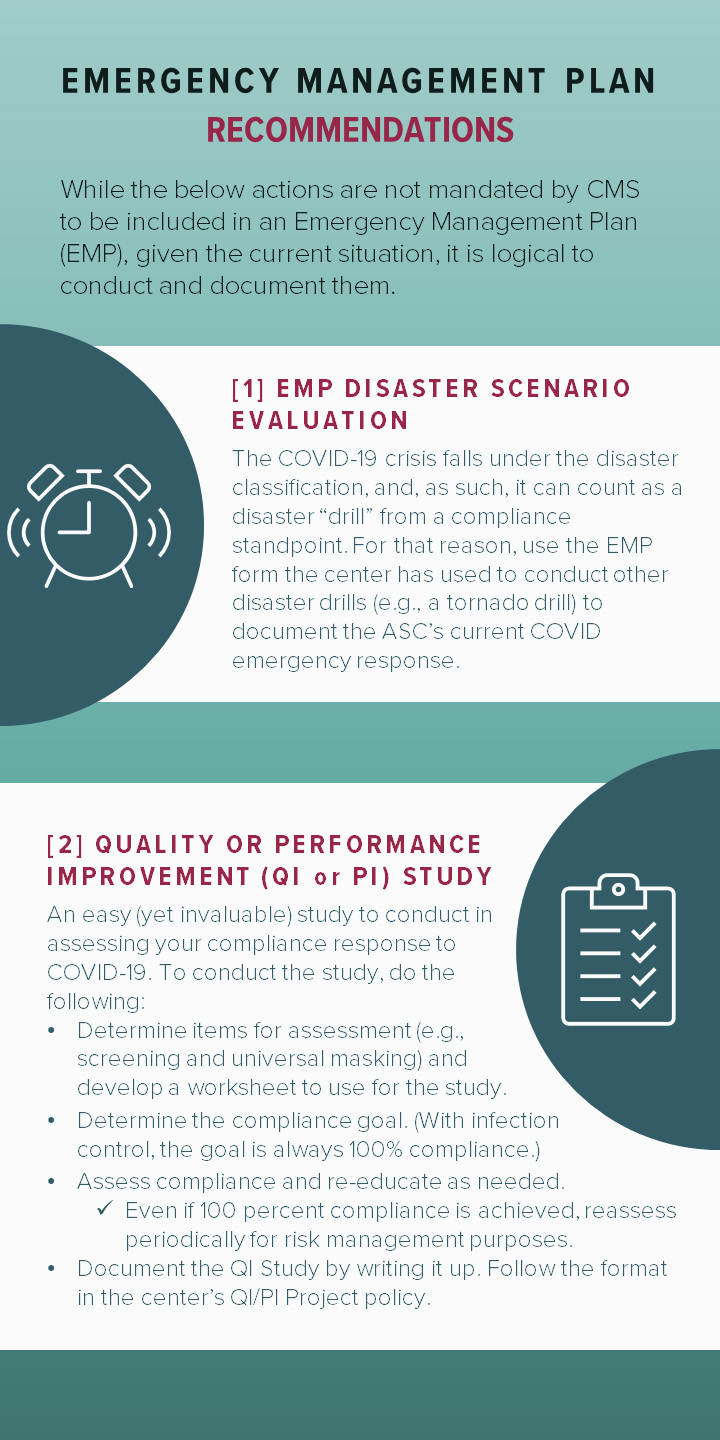
Per the Centers for Medicare & Medicaid (CMS) Conditions for Coverage, all ASC facilities must have a Disaster Preparedness Plan, also known as an Emergency Management Plan (EMP). An EMP must include measures in each of these four major areas: Risk assessment and planning, policies and procedures, communication, and training and testing. The current pandemic has already required changes be made to an ASC’s EMP; therefore, it is important that those changes be clearly memorialized. Let’s take a closer look at each of the EMP’s four areas to see what updates to consider and document.
Risk Assessment and Planning
CMS requires centers to have their EMP based on an “all-hazards” approach, or one that focuses on preparedness for a full spectrum of emergencies or disasters. Consider all hazards through the following annual evaluations:
- Hazard Vulnerability Analysis (HVA). This provides a straightforward way to complete a risk assessment and the potential impact of multiple hazards. Among those hazards to consider are emerging infectious diseases. CMS added that requirement in response to previous Zika and Ebola outbreaks. Enter the COVID-19 pandemic, which is considered a much higher threat to facilities than Zika or Ebola previously. In response, centers must update their HVA to reflect the risk of this pandemic and change it as needed.
- Infection Control Risk Assessment (ICRA). Update this existing center assessment to include COVID-19 and facility actions surrounding it.
Policies and Procedures
The policies and procedures in an EMP must be based on the center’s HVA; risk assessments; and local, state, and federal regulations. A center’s EMP may either be in a separate binder or part of its general policies and procedures, depending on state requirements. For purposes of this discussion, we are including “Updating your EMP” in the policies and procedures section.
- Updating your EMP. Review the center’s current plan and consider adding the following information due to COVID and its impact:
- Financial stability: Include information and planning around business office functions (e.g., accounts receivable/accounts payable (AR/AP), service contracts, and deposits) along with the need for cash projections in the EMP.
- Supply shortages: Have a plan for long-term supply shortages in light of current personal protective equipment (PPE) shortages.
- HR: Prepare for furloughs and layoffs and how to carry them out when planning for reduced operations or a shut down. Also, plan to recruit when attempting to bring staff back once operations ramp up or resume.
- Community needs: Consider the center’s provision of PPE, anesthesia machines, and other resources in relation to local hospital needs.
- Additional policies. While infectious diseases may have been eluded to in previous policies and procedures, COVID-19 presents additional items that require policy development. They include:
- Appropriate use of PPE
- Environment of care, including non-patient care areas (e.g., lobbies and lounges)
- Intubation/extubation for COVID-19
- Post-exposure plan for COVID-19
- Screening of patients, employees, and medical staff
- Social distancing
- Universal masking
- Visitor protocol
- A Respiratory Protection Program
Communication
Clear and upfront communication is necessary with staff, patients, visitors, and licensed independent practitioners (LIPs)/allied health professionals to ensure safety. Relay recent changes to everyone, including the center’s governing body for review/approval. Items to get board approval on include delegations of authority (administrator for the Respiratory Protection Program); new cleaning products; updates to the HVA, ICRA, and EMP; and policies and procedures. It’s important that everything is reviewed and approved through the proper channels, as this ensures that documentation exists for any future review.
Training and Testing
As with all new policies and practices, training and testing must occur. This is the most important factor in achieving compliance. Educate LIPs, staff, patients, and visitors — essentially anyone entering the ASC — on the center’s latest COVID-19 protocols. To ensure compliance, do spot checks to gauge adherence to the latest rules. From those, next steps to reach total compliance can be crafted and implemented. The alternative is to risk a COVID-19 exposure/outbreak in the center.
An Ongoing Effort
The saying in the compliance world is that “if it wasn’t documented, it wasn’t done.” Make sure to take credit for recent efforts by properly documenting them. The twist and turns of this virus will most likely provide ample opportunity to continue making facility policy and procedure changes. Be sure to capture those updates on paper.
HELPFUL RESOURCES: To help ASCs navigate their reopening and operations efforts, Progressive Surgical Solutions recently created COVID-19 toolkits. The COVID-19 QAPI Toolkit contains everything you need to document your emergency response. Purchase the kit on Progressive’s COVID-19 Information Hub.